If you’re in the medical billing business, you know all too well that customers aren’t always trusting of the billing process. We’ve all been in the shoes of a patient waiting to see how much insurance covers, what we’ll have to pay out of pocket, and other financial situations that can become a burden. Sometimes it’s hard to trust a process that you can’t see or don’t feel is transparent. That’s why we’re breaking down some common myths surrounding medical billing—how does it work? What do medical billers do? Where do these numbers come from? If you’re skeptical of the process, read on for a new perspective on medical billing.
Myth #1: Billers Only Need Limited Medical Knowledge

Nope, not even close. In fact, medical billers need a wide host of not just medical knowledge, but experience with insurance policies, HIPAA regulations, coding guidelines along with math and organizational skills. These professionals have to read detailed, lengthy medical reports each day, which they must then be able to understand and translate into a useful document.
Myth #2: Billers and Coders Mostly Enter Data All Day Long

There’s a lot more to these jobs than data entry. Everything that happens before the data can be entered into a system is the hard part of these jobs. Billers need to be familiar with a variety of insurance companies’ policies and ensure that they have the correct information, service performed, and insurance information from the patient. Coders then have to take that information and decipher it, deciding what is relevant and translating it into universal codes for insurance submission.
Myth #3: Billers’ Jobs Will Become Obsolete Because of Technology
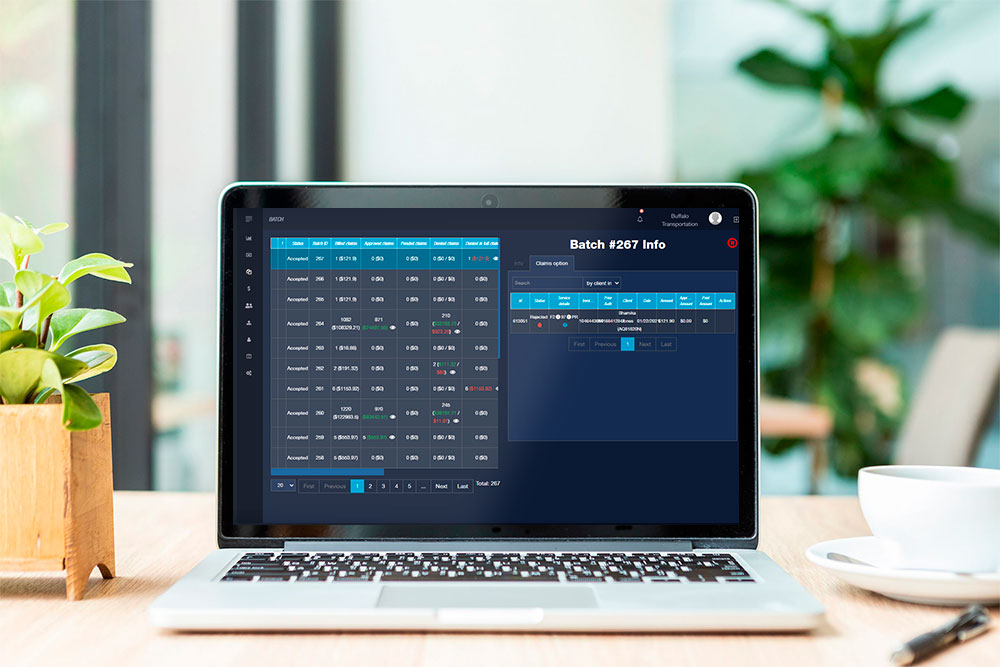
If we’re being honest, we’ve all considered the possibility of being replaced by computers at our jobs. There’s no saying the grand sci-fi movies aren’t on to something, but for now, technology is more of a help than a threat. For instance, NY Medicaid billing software is an extremely useful tool that more and more billing companies are turning to for assistance. It makes the process quicker and more efficient, but it doesn’t eliminate the need for real people. Billers are still the ones who gather and sort through information. Plus, when it comes down to it, technology still leaves room for error. So, no, medical billers aren’t being replaced by technology anytime soon.
Myth #4: Medical Billing and Coding is Easy

This assumption comes from the idea that a person sitting at a computer all day must have a fairly easy job. Medical billers aren’t the ones meeting with patients face-to-face or physically performing check ups, but they’re still working in the medical field. Medical billers and coders have to have an in-depth understanding of the human body in order to translate diagnoses into codes for billing.
A Fresh Perspective

If you’re already working in the medical and healthcare industries, none of these myths should have surprised you. But if you’ve experienced people who are hesitant toward trusting medical billers, or you yourself have felt unsure of the transparency of the process, we hope you gained a new perspective here. The team at BillPro would love to get in touch if you’re in the market for Medicaid billing software. Feel free to contact us with any questions or inquiries you have, anytime!
 0/5 (0 votes)
0/5 (0 votes)
 189 views
189 views




