Medical billing is a complex process, often made easier with the help of NY Medicaid billing software. Billing is necessary in all aspects of healthcare and ensures the customer pays for their service, through insurance or private pay, and that providers are reimbursed properly. Software or not, the process is always the same. There are 10 general steps that make up the medical billing cycle—used at hospitals, doctors offices, rehabilitation centers, specialists’ offices, and more. The details of the process may differ from office to office, but these medical billing cycle steps are, in one way or another, the universal guide to the medical billing workflow.
Patient Registration

It shouldn’t be a surprise that the first step of the medical billing cycle occurs at the very beginning of an appointment, or sometimes even before the appointment. Office staff collects basic information about the patient including name, date of birth, address, reason for their visit, and more. They also take down insurance information including provider and policy number, so they can quickly confirm the information is accurate. This part seems easy, but it’s a crucial first step. If incorrect information is written down during registration, it can become a problem later down the line of the billing cycle and can even cause errors in claims if not fixed.
Confirm Financial Responsibility

This step consists of a deeper look into the patient’s insurance coverage. The staff carefully looks over insurance information, seeing whether the patient’s requested services are covered through their provider. If there’s anything insurance won’t cover, the patient is informed that they’ll be financially responsible for those costs.
Create the Superbill

Once the appointment is finished and you have all valid patient information including insurance, identification, and co-payments, it’s time to create the “superbill.” This report consists of all existing information from both the registration and the appointment, plus the diagnosis and billing codes.
Generate the Claim

By this point, you have all the necessary information to create a medical claim for the insurance company. Once a claim is created, it’s crucial to ensure information is correct and no coding or billing errors are present. This is a simple check if you’re using Medicaid billing software for your claims. The software will automatically check for errors before submitting, so you don’t have to worry about mistakes coming back later on.
Submit the Claim

Once you’re confident the claim is free of errors, it’s time to submit to the insurance provider. Depending on whether you’re billing manually or electronically, this part of the process will vary slightly. If you’re manually submitting, you’ll probably take a pile of claims to the post office all at once. When you’re using automated billing software, it’s easy to send each claim instantly. Electronically billed claims will be paid first, so if you’re still on the fence about using software, that’s something to consider.
Monitor Claim Status

At this point, you’re going to experience a wait period. During this time, the payers look over your claim, checking that the information is valid. Once they’ve assessed the claim, there could be a few different outcomes: your claim is accepted, and you’ll be reimbursed; your claim is rejected, and you’ll have to fix errors and resubmit; your claim is denied, and you’ll have to fix the errors, if possible, and resubmit.
Create the Patient Statement

After the claim has been processed, it’s time to bill your patient for any outstanding charges. This statement will include the total cost, including what services insurance covered and how much they paid, along with what services they didn’t cover and the amount the patient owes.
Patient Follow-Up

This step may or may not be necessary, depending on whether your patient pays their bill in time. If you don’t receive a payment by the due date, you’ll have to send a follow-up statement. If you don’t receive payment or a response after that, it may be necessary to contact a collection agency.
Do Better Medicaid Billing With NY BillPro
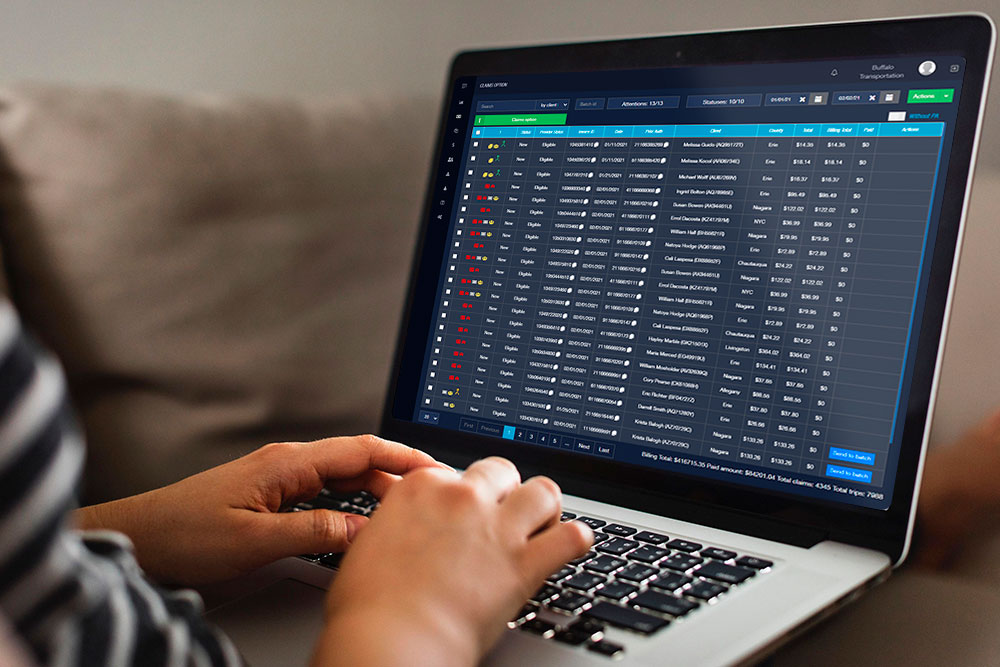
The medical billing process is more or less the same at most practices. But how to choose to complete the process—by manually filing claims or submitting them electronically—makes all the difference. If you’re ready for a more efficient, seamless Medicaid billing process, get in touch with our reps at BillPro. They’ll be happy to schedule a demo with you, where you’ll get an inside look at the Medicaid billing software in action. Plus, you’ll have the chance to ask any questions about the software and how it relates to your business. Don’t settle for slow, faulty billing. See what BillPro can do for your business today.

 2.3/5 (3 votes)
2.3/5 (3 votes)
 908 views
908 views




